16) In retrusive position, the lower incisors should not
be within
2 mm of the distal edge of the DE. If so, gradual resolution of
the patient's myofascial condition may allow for an improved
range of motion, thereby allowing the patient to "bite behind
the bump". (methylmethacrylate is easily adapted on the DE
to enhance it).

17) Although the angle of the DE is close enough to perpendicular
to the
long axis of the lower incisors (where intense clenching does no trauma),
the slope of the DE in #17 above allows for resistance to protrusive/superior
force (red arrow) when the mandible protrudes. The patient's temporal
symtoms may decrease, but facial (lateral ptyergoid) and cervical
(trapizus) symptoms may persist or intensify. (Remedy: Level the
DE
parallel the maxially occlusal plane)


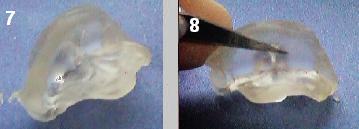
18 and 19: "Getting in Front of the Bump") If the
patient can protrude
and place the lower incisors anterior to the labial edge of the DE,
it should
lengthened (below) so that in maximum protrusion, the incisors
are always contacting
the DE (close to) their long axis. (To confirm whether or not
the patient is
actually "getting in front of the bump", ask them to do it while in
the office.
If it is uncomfortable, or painful, chances are that they are.)
Facial and TMJ pain typically result if left un-modified.